Estrogen therapy
Estrogen-only HRT with or without anti-androgen therapy is the mainstay of feminising hormone treatment for trans women wishing to medically transition.
Some (but by no means all) non-binary people assigned male at birth (AMAB) opt for low dose estradiol therapy under specialist guidance.
Preparations considered to have the safest risk profile include estradiol valerate and estradiol hemihydrate. The more pro-thrombotic agents including ethynylestradiol and conjugated equine estrogens (for example, Premarin) are now contraindicated and should not be prescribed.
In the UK, there is no role for the use of progestogens in this context. Combination HRT is associated with a higher risk of thrombosis2, cardiovascular disease3, and breast cancer4, and there is currently insufficient evidence that progestogens convey additional benefits with regard to breast development.
Estrogen is titrated slowly with the usual aim of bringing about the changes associated with female puberty. The aim of treatment in this context is to produce a blood serum estradiol level in the range 350-750pmol/L*.
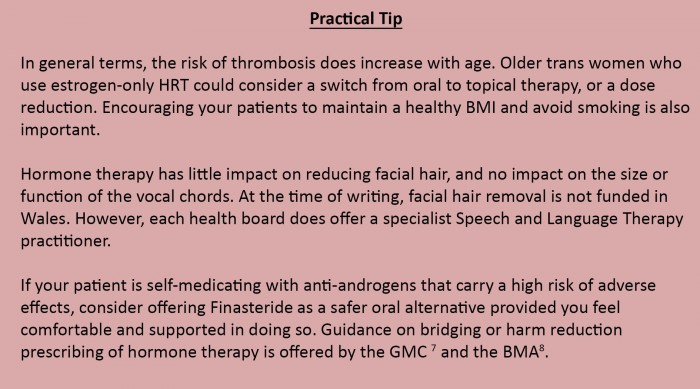
Oral routes of administration are more thrombogenic due to the “first pass effect” than are transdermal routes, and the risk of thromboembolic events is dose-dependent.
Topical HRT is associated with a lower risk of thrombo-embolism5 and can be a first-line option, particularly for people over the age of 40, people with obesity, and in those who continue to smoke.
Most people use hormone replacement therapy (HRT) lifelong unless medical complications arise. Compulsory discontinuation with advancing age is not justified. In the event of medical complications such as thrombosis, stroke, ischaemic heart disease or a cancer diagnosis, specialist advice should be sought.
Studies in older adults are lacking, but in the case of those wishing to reduce their dose at menopausal age, maintaining serum estradiol of around 200pmol/L is broadly considered to offer sufficient bone protection and maintain feminisation.
DEXA scanning tends to be reserved for people at higher risk of osteoporosis and is not routinely recommended. However, Ca/Vitamin D supplementation is often encouraged as Vitamin D deficiency appears to be common in this group.
Anti-androgen therapy
In addition to estrogen therapy, most trans women who require testosterone suppression will need anti-androgen medication in order to achieve this. In the UK, this usually takes the form of a GnRH agonist injection. A GnRH agonist briefly stimulates, then down-regulates the release of FSH and LH from the pituitary gland, reliably shutting down gonadal testosterone production such that routine serum testosterone measurement is not required. This treatment is typically introduced a little while after estrogen therapy has started in order to mitigate menopausal symptoms and bone mineral density loss.
GnRH agonists are for the most part very well tolerated and are a pre-requisite to genital surgery in order that the patient can experience the castrate hormone milieu in a reversible way. A small number of patients report a loss of sexual fantasies and desire for sexual activity (features of hypoactive sexual desire disorder) and may require specialist guided add-back testosterone replacement
A GnRHa injection will bring testosterone into the female range 0-3nmol/L
One oral anti-androgen alternative is Finasteride. This blocks testosterone conversion to the more potent DHT (dihydrotestosterone), and, while far less effective as an anti-androgen, it can be a preference for people assigned male at birth not wanting or requiring full testosterone suppression (for example in those wishing to preserve some erectile function) and for those wishing to protect their scalp from further hair loss
Some (but by no means all) non-binary people assigned male at birth (AMAB) opt for anti-androgen monotherapy under specialist guidance
Spironolactone (Aldactone) and Cyproterone acetate (Androcur, Cyprostat, Dianette) are two anti-androgens commonly purchased on the internet for the purpose of self-medication. Spironolactone affects electrolyte balance, is diuretic, and appears to have a negative impact on breast development. Cyproterone acetate is associated with hepatic dysfunction and depression 6. They are not routinely used in the UK in this context*
* The target range recommended in ‘Hembree WC, et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism, Volume 102, Issue 11, 1 November 2017, Pages 3869–3903’, is 100-200pg/ml (367-734pmol/L)
* Cyproterone acetate 100mg OD is used as a short-term treatment to counteract the testosterone flare that follows the first GnRH agonist injection.