Testosterone therapy
Testosterone therapy
Testosterone therapy is usually titrated gradually, starting with a gel or short-acting injectable formulation, and moving on to a long-acting injection in accordance with patient preference.
The aim for most trans men is to achieve a serum testosterone level equivalent to the adult male range. Some (but by no means all) non-binary people assigned female at birth (AFAB) opt for low dose testosterone gel therapy under specialist guidance.
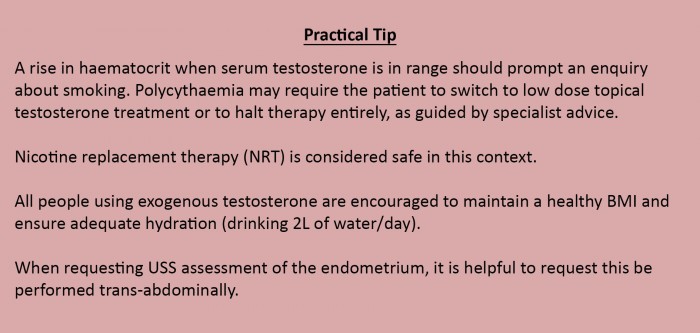
Testosterone stimulates erythropoietin production and therefore increases the risk of secondary polycythaemia. This is defined as haemoglobin > 185 g/l and/or HCt > 0.52.
Smoking also causes erythrocytosis and is associated with plasma volume contraction, which leads to hyperviscosity. It can also impact negatively on surgical outcomes, particularly of free graft survival (for example nipple relocation during chest surgery, and radial forearm or thigh grafts in phalloplasty).
Sustanon is the most commonly used short-acting injectable testosterone in the UK. Due to the greater fluctuation in serum testosterone levels with this preparation, some people experience a more labile mood, and in this context, gel applied daily offers more control and less variability.
There is some evidence that Sustanon and other short-acting preparations are associated with higher rates of polycythaemia (up to 40%)9 than the long-acting injectable Nebido (around 11%). Nebido or testosterone gel tend to be the preferred long-term options.
Transmasculine people using testosterone are eligible for gamete preservation but should receive counselling regarding the potential risks and uncertainties surrounding the impact of exogenous androgen exposure on fertility, fecundity and foetal development.10
Previous studies reported endometrial proliferation in approximately 15% of patients on long-term testosterone treatment. However, this evidence is being challenged and there is less emphasis on hysterectomy. Current recommendation is for biennial ultrasound assessment of the endometrium starting after 2 years of testosterone therapy.