Ulcer assessment
Thorough assessment is needed to identify underlying venous disease with the aim of treating the disease along with the ulcer and to rule out an alternative diagnosis
EWMA Statement 5.2a: All patients presenting with lower leg ulceration must receive a comprehensive assessment. In England the national wound care strategy program has published a minimum data set that has to be assessed in patients with VLU
(http://www.ahsnnetwork.com/wp-content/uploads/2019/11/V2-Draft-Lower-Limb-Assessment-Essential-Criteria-25.11.19.pdf) accessed 19th October 2020.
- Assess the site of the ulcer. Venous ulcers are typically situated below the knee and above the ankle (this area is known as the gaiter area) and around the inner and outer malleolus. Venous ulcers are usually shallow with gently sloping, irregular edges. Check for any undermining, rolled or raised edges as this may indicate a possible malignancy (Marjolin’s Ulceration) and a biopsy should be taken for histological examination (Young 2020).
- Record details about the ulcer, such as the size and depth. If possible, and with written consent take a photograph of the ulcer.
- Note the type of tissue on the wound bed
- Granulation tissue is red, healthy tissue

- Hypergranulation/overgranulation tissue can be seen as over granulating or proud flesh that extends vertically above the level of the surrounding skin, this will require flattening to enable reepithelialisation and the covering of the granulation tissue by new epidermis, topical steroid therapy can be used to reduce the hyper/over granulation as a short term intervention.

- Epithelializing tissue are tightly packed cells that grow over granulation tissue to restore the epidermis. They are pink in colour and can be seen at the wound edges or as white/pink islands in the wound bed where they are generating from hair follicle sites. This tissue is evidence of healing

- Slough this is non-viable tissue which can be soft or hard and wet or dry and is usually yellow in colour

- Necrotic tissue presents as black or brown in colour and this is non-viable tissue.
- Infected tissue tends to be green in colour (or could be bright green if Pseudomonas Aeruginosa is present). Document the percentage of each tissue type in wound which will allow for monitoring improvement or deterioration in the wound bed.

- Signs of infection include an enlarging ulcer accompanied by a changing, new or foul odour and there may be increased pain or exudate. A localised infection will be contained within the wound bed/peri-ulcer skin, whereas a cellulitis is an infection that is seen to be spreading up the limb. NICE have issued guidance on cellulitis and antimicrobial prescribing (NICE 2019)
- Assess for peripheral vascular disease (this has to be done prior to the commencement of compression therapy) - assess for, pallor, coldness and dusky appearance on the lower leg, capillary refill (>4 seconds is indicative of arterial insufficiency).
- Inspect the peri-wound area to assess for maceration, cellulitis, oedema, erythema, or varicose eczema.
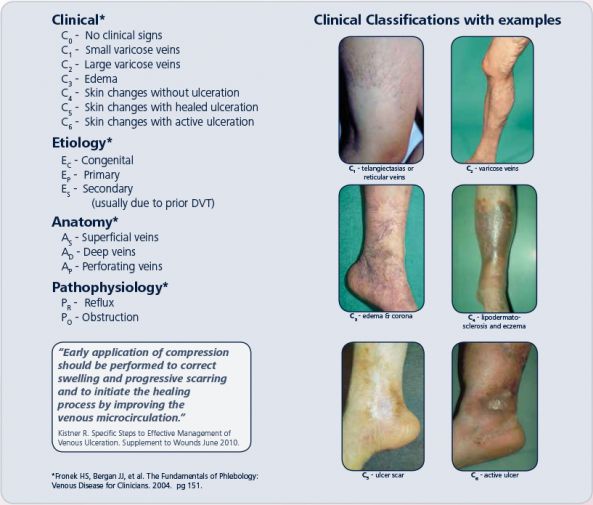
The following is the EWMA recommended classification of venous disease